Navigating the "Homebound" Requirement for Home Health Agencies
The homebound requirement is the bedrock of Medicare's home health benefit. Simply put, it's one of the core criteria that must be met for a patient to receive skilled care in their residence. For home health agencies, accurately and consistently documenting the homebound status isn't just a regulatory hoop—it's essential for ensuring appropriate care and justifying reimbursement.
But what exactly does "homebound" mean, and how do you keep your documentation consistent throughout an episode of care? Let's break it down.
Understanding the Two-Part Homebound Criteria
Medicare defines "homebound" with two main criteria, and the patient must meet both:
Criterion 1: The "Why"
The patient must need one of the following to leave their home due to illness or injury:
The aid of supportive devices (crutches, canes, wheelchairs, walkers).
Special transportation (e.g., medical transport).
The assistance of another person.
Alternatively, they have a condition where leaving home is medically contraindicated (e.g., severe immunosuppression).
Criterion 2: The "Effort"
There must be a normal inability to leave home, and leaving requires a considerable and taxing effort.
It's important to remember that "homebound" doesn't mean "house arrest." The patient is still allowed to leave for medical treatments (like dialysis or physician visits) and for infrequent, short-duration non-medical reasons (like religious services, an occasional trip to the barber, or a family event). The key is the considerable and taxing effort involved in those outings. If a patient can easily get out and about, they are not homebound.
Documenting Consistency: Tips for Clinicians
Consistency in documenting the homebound status is crucial from the Start of Care (SOC) to discharge. Your visit notes should reinforce the same clinical picture that was established during the initial assessment.
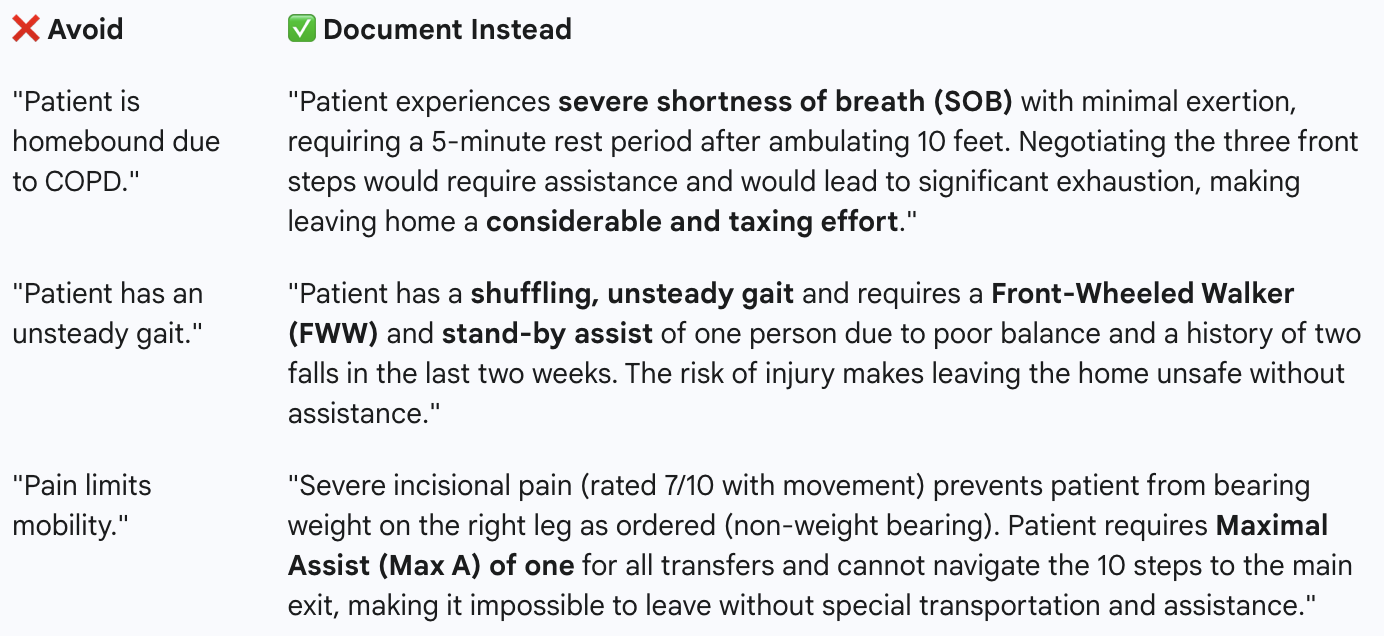
1. Be Specific and Objective
Avoid generic statements like "patient is weak" or "patient has SOB." Instead, paint a vivid, objective picture of the functional limitations and the effort involved in leaving the home.
2. Connect the Skilled Need to the Homebound Reason
Your documentation should clearly illustrate how the skilled service you're providing is directly related to the illness or injury that makes the patient homebound. For example, if a patient is post-op from a hip fracture, the need for skilled physical therapy to regain ambulation ability (skilled need) is intrinsically linked to their inability to safely mobilize and leave the home without assistance (homebound reason).
3. Report Absences Realistically
If the patient leaves the home for an allowed reason (like a doctor's appointment), your note shouldn't just say they went out. It should reiterate why the trip was still taxing and supported the homebound status.
Example Note Excerpt:
"Patient attended their follow-up cardiology appointment today. Per caregiver report, the patient required wheelchair transport from the car to the office and was visibly exhausted upon return, needing to rest in bed for 2 hours post-visit. Leaving the home continues to require a considerable and taxing effort."
When and How the Homebound Reason Can Change
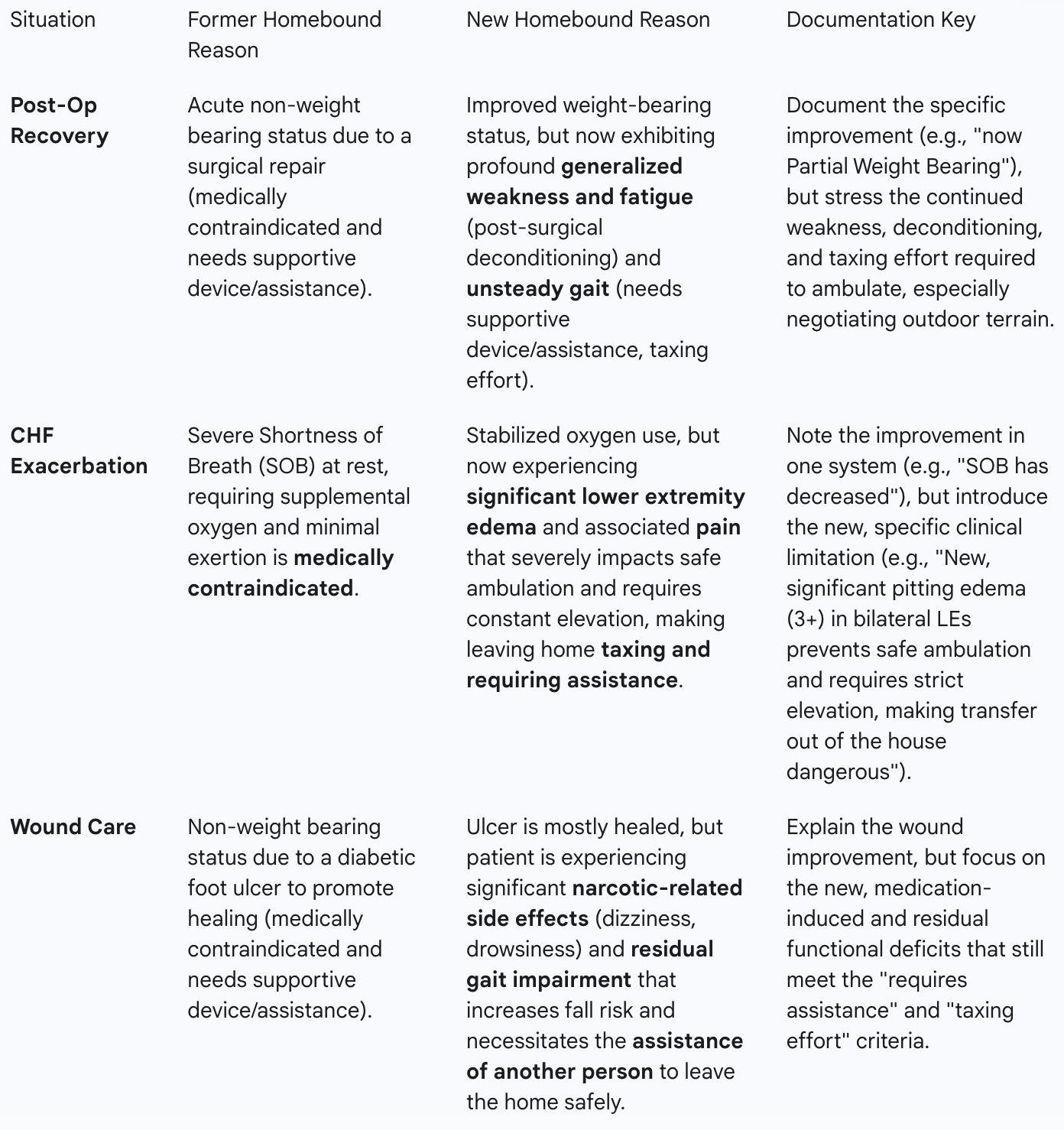
A patient's clinical condition isn't static, and neither are their reasons for being homebound. It's perfectly normal—and expected—for the specific clinical factors supporting the homebound status to evolve during a 60-day episode.
Documenting a Change
When a clinical parameter improves or another limitation emerges, you must document the change and clearly articulate the new reason that supports the continued homebound status. This is a critical point for demonstrating consistency: the underlying status is the same, but the clinical justification may have shifted.
Example Scenarios:
By being hyper-specific, objective, and intentional in your visit notes—always tying the current clinical picture back to the two-part criteria—you provide the comprehensive, consistent narrative that ensures compliance and supports the excellent care you're providing to those who truly need it most.